Women being misdiagnosed as health issues ‘not taken seriously’

Women in the UK are at risk of being misdiagnosed or given the wrong medication as more than half (60%) say their health issues are not taken seriously by healthcare professionals.
In a survey of 10,000 UK women aged 16 and over, more than a third (35%) of women said they have experienced poorer health outcomes because of their gender.
The survey, carried out by healthcare provider Benenden Health as part of a campaign with the Fawcett Society and TV presenter Cherry Healey, also found that 35% of respondents said they avoid going to the doctors because of anxiety and embarrassment, among other reasons.
Of the women who said they have experienced poorer health outcomes, a third (33%) said they have received an incorrect diagnosis, while a quarter said they have been put on the wrong medication at some point in their lifetime.
Among this group of women, more than half said they had a negative experience with healthcare professionals and over a third (36%) said they received a late diagnosis for their illness.
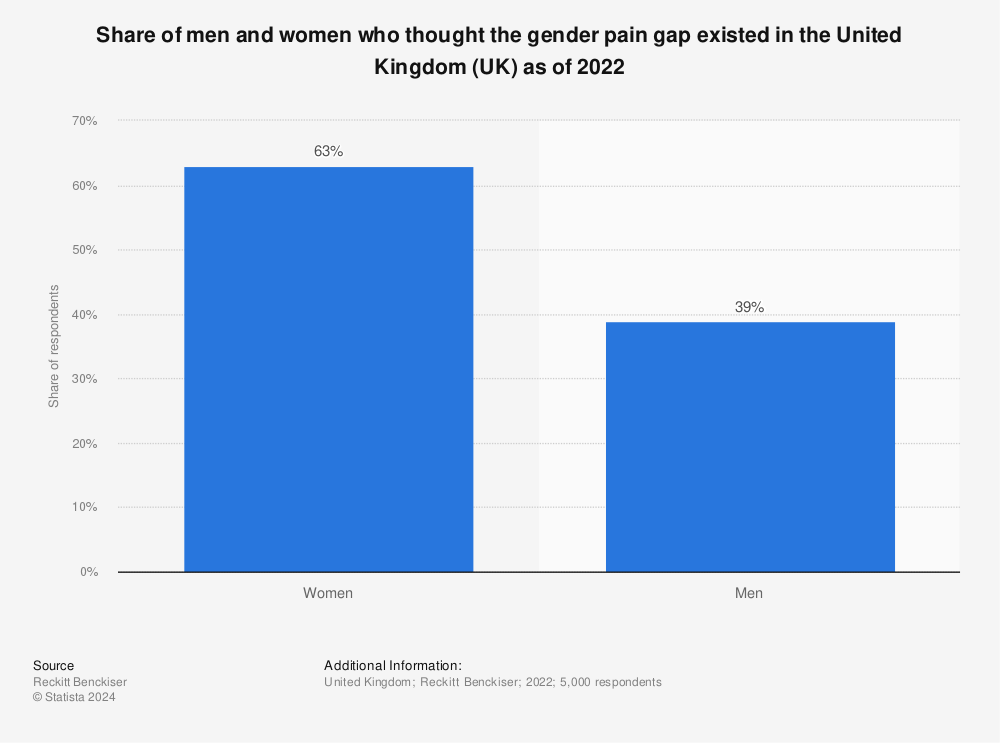
The campaign between affordable private healthcare provider Benenden Health, the Fawcett Society and Healey aims to highlight the impact of the UK’s "gender health gap" - which is the largest among G20 countries and the 12th largest globally.

While in many countries, men are more likely to face greater health risks than women, the UK’s gender health gap is known to result in worse medical treatment for women.
In 2022, the Department for Health and Social Care (DHSC) said that its call for evidence to inform the government’s first Women’s Health Strategy revealed that more than four in five (84%) of respondents said they, or women they know, were not listened to by healthcare professionals.
Many said their symptoms were "not taken seriously or dismissed upon first contact with GPs and other healthcare professionals", and they had to "persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years".
Benenden Health’s survey also revealed that more than a quarter (27%) of women feel the UK’s healthcare system favours men over women. Many are left feeling reluctant to seek medical help at all, which further impacts their long-term health.
Rowan Connell, medical director and consultant gynaecologist at Benenden Health, said that the findings "paint a concerning look at women’s health in the UK, but it’s a reality that, as a society, we cannot shy away from".
Jemima Olchawski, chief executive of the Fawcett Society - which is the UK’s leading charity for gender equality and women’s rights - added: "Research like this shows just how much work there is still to be done in even just beginning to understand how stark inequality is in the UK today, and in ways that can seem ‘invisible’.
"It’s time for change. The current system doesn’t work for anyone: women are being let down and the cost to business is enormous.
"We hope some of the clear solutions offered in this research will encourage employers and government to step up to the challenge and build a system that works better for women, in order to begin closing the Gender Health Gap."
The charity shared the stories of six women whose health has suffered as a result of the gender health gap.
In one story, a woman named Genny said her hair began falling out after she went on a hiking holiday to Turkey, where she was bitten by an insect and got a "strange mark and a fever".
Her GP was initially "very patronising", she said, and "dismissed" her symptoms as her having a "dry scalp". However, Genny’s condition deteriorated to a point where she had to sign off work for two-and-a-half months due to "severe fatigue", "intense night sweats and memory loss".
She was finally diagnosed with Lyme disease - but the diagnosis only came after months of feeling unwell and yet another negative encounter with a healthcare professional.
Another woman named Jodie said it took her nearly two decades to get a diagnosis of endometriosis.
Before her diagnosis, she endured excessive bleeding and pain during her periods. Jodie said her family doctor’s response when she was 11 was to say this was "what all the women in your family go through" and she was put on contraception.
Jodie became pregnant unexpectedly and while her son was very welcome, pregnancy made her body feel like it was "being torn apart". After the birth, a specialist consultant for endometriosis told her "having another baby would cure my condition, which is just not true".
Healey, who is a women’s health advocate as well as a regular presenter on BBC Two’s Inside The Factory, said of the survey: "This campaign is so important in the fight to enable women to talk more openly about their own health, so that when they express their health concerns, they are taken seriously.
"This is an issue that I feel very strongly about, having previously shared my own experience of perimenopause and learning about the avoidable challenges so many women go through to get the help they need. I want to help ensure that women all over the UK are receiving the support that they need, when they need it."
Watch: Closing 'gender health gap' could add $1T to global GDP: Study
Read more about women's health:
Dentist reveals why women experience more teeth issues than men (Yahoo Life UK, 5-min read)
Vaginal discharge and a low libido among conditions women are embarrassed to discuss (Yahoo Life UK, 6-min read)
Menopause made my insides 'fall out' – women should be taught how to stop this happening (Yahoo Life UK, 11-min read)


