Where measles has spread the most, mapped
A “call to action” is needed across the country for parents to get their children vaccinated against potentially deadly measles.
That’s the view of Prof Dame Jenny Harries, chief executive of the UK Health Security Agency (UKHSA), amid warnings that measles is spreading among unvaccinated communities.
It comes as vaccination rates across the country have been dropping, with Prof Harries saying on Friday: “I think people have forgotten what measles is like. I’m actually [from] the generation that had measles… I can remember it and it is miserable.” Mortality is “relatively low” but measles can nonetheless have “serious” health consequences, she warned.
Here, Yahoo News UK explains where and why it is spreading.
Where are the hotspots?
Figures released by the UKHSA show there have been 216 confirmed measles cases and 103 probable cases in the West Midlands since 1 October last year.
Four-fifths (80%) have been found in Birmingham while 10% were identified in Coventry, with the majority being in children aged under 10.
Separate UKHSA statistics show there were 209 laboratory-confirmed cases of measles in England between January and November last year. Of these, 50% (104) were in London, with 26% combined in the West Midlands and Yorkshire (28 and 27 cases). Of that 209 total, meanwhile, 59% (123) were among children under 10.
How quickly does it spread?
Prof Harries warned on BBC Radio 4’s Today programme that measles “is the most highly infectious virus of all respiratory illnesses we deal with routinely”. It has a reproduction (R) number of 15 among unvaccinated populations, Prof Harries said. This means each infected person would theoretically infect 15 more people in such an instance.
For context, Prof Harries pointed out the R number for COVID during the lockdown years of 2020 and 2021 was around 1 or 2. “People might find that quite alarming and see why this is important," she added.

Vaccine take-up concerns
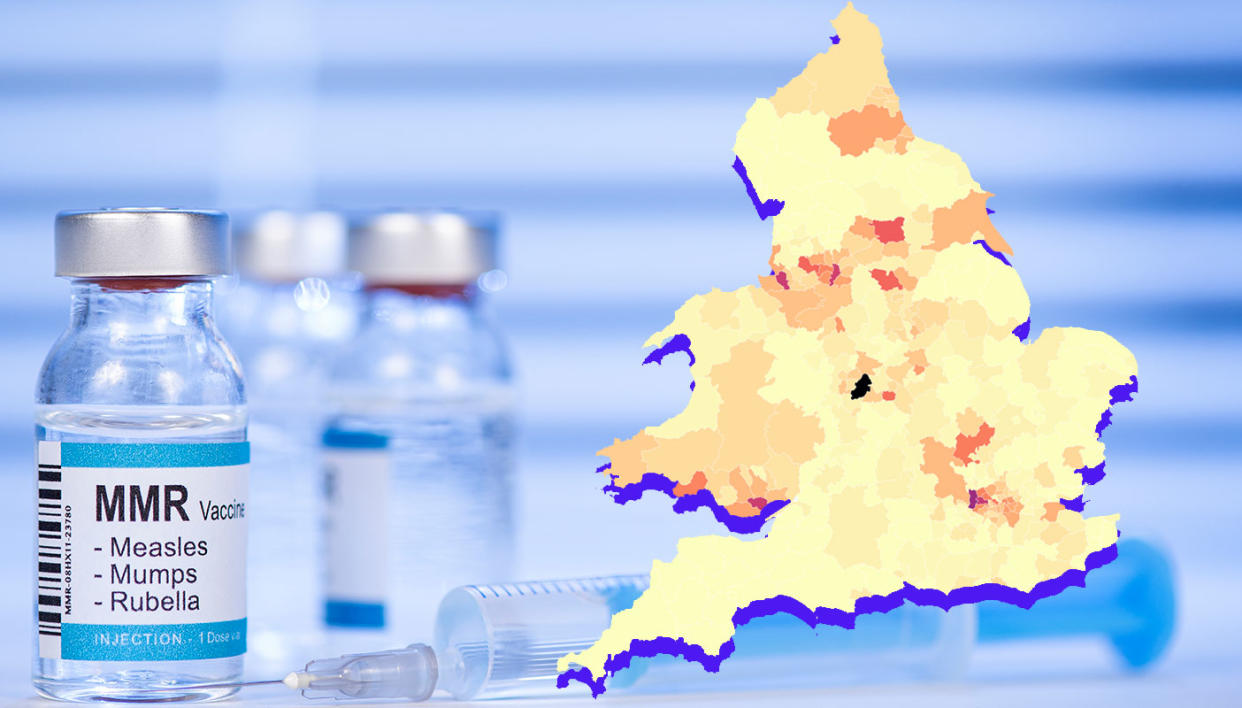
Vaccination rates across the country have been dropping, but there are particular concerns about some regions, including parts of London and the West Midlands.
In 2022/23, 84.5% of youngsters in England had received both doses of their MMR (measles, mumps & rubella) jab by the time they were five years old, the lowest level since 2010/11. The World Health Organization recommends a target of 95%, with Prof Harries admitting the vaccine programme in the UK is “clearly not” where the UKHSA needs it to be.
Where are the lowest vaccine rates?
According to NHS England figures from 2022/23, the five areas with the lowest proportion of children to receive both doses of their MMR vaccine by their fifth birthday are all in London. They are:
Hackney & City of London: 56.3%
Camden: 63.6%
Enfield: 64.8%
Haringey: 65.9%
Islington: 66.3%
For context, the East Riding of Yorkshire had the highest take-up with 94.4% - and even this is below the 95% target figure.
What are some of the reasons?
Ronny Cheung, a top children's doctor, thinks a lack of knowledge is to blame as much as vaccine hesitancy for lower take-up.
Dr Cheung, officer for health services at the Royal College of Paediatrics and Child Health, told the PA news agency earlier this week: “Whilst there is still a bit of hesitancy around, actually there are also a significant number of people who say they didn’t know that they could get catch-up vaccines or they don’t know where to go if they have missed that.
“I think we have a lot to do in terms of signposting people to the right place to access it as well rather than just blaming it on vaccine hesitancy.”
Dr David Elliman, community paediatrician at Great Ormond Street Hospital, said there should be two priorities for health authorities: first to "ensure that parents know when their child should be immunised and make it easy for it to be done" and second "to recognise that parents understandably have questions about vaccinations, possibly more since COVID. Most, given time to talk to a trusted healthcare professional, will be reassured".
Read more
Map reveals where measles cases are surging across the UK(The Independent)
Measles signs and symptoms to look out for as UK cases rise (Yahoo Life UK)
People have ‘forgotten’ the risks of measles, top children’s doctor says (PA Media)
Which demographic groups have low take-up rates?
Prof Harries acknowledged uptake of MMR vaccines does differ among communities.
Asked which communities, she said: “This is an important point, I think, for the West Midlands. For those in Muslim communities, they will be not keen to take up one of the MMR vaccines that we offer which has a pork-based derivative. But it’s really important that they’re aware there is a non-porcine vaccine which is available to them and very effective."
Echoing the comments of Dr Cheung and Dr Elliman, she emphasised the need to ensure "knowledge is available to people so they can make choices".
In terms of age range, there are also concerns around the take-up among young adults - the 1998-2004 birth cohort - who are beginning to enter the workplace and whom the UKHSA is keen to presuade to get catch-up jabs.
What are the symptoms?
According to the NHS, measles usually starts with cold-like symptoms including a high temperature, a runny or blocked nose, sneezing, coughing and red, sore, watery eyes. This is followed by a rash a few days later, starting on the face and behind the ears before spreading to the rest of the body.
Read more: Measles signs and symptoms to look out for
What are the potential complications?
Helen Bedford, professor of children’s Health at the UCL Great Ormond Street Institute of Child Health, outlined why measles is a "potentially very serious infection".
"At best," Prof Bedford said, "measles makes people feel very ill with a high temperature, sore eyes, a cough and a rash. However, it also can lead to complications including ear infections, pneumonia and fits. About one in 1000 people with measles develop inflammation of the brain (encephalitis) and even in high-income countries like the UK, about one in 5,000 die from the infection."
She added measles is "often more severe in adults" and that there is no treatment "apart from managing the symptoms".
There are also social impacts to consider, with children required to take time off school and parents time off work to look afetr them


