Is it time to treat COVID like other viruses?

When first lady Jill Biden tested positive for COVID-19 earlier this week, it publicly confirmed what many Americans have already picked up on in their personal lives.
The virus is back — again.
Though official case counts tell only a sliver of the story, it’s clear that the U.S. is experiencing another mini-wave of infections.
But wait: Wasn’t COVID supposed to be behind us?
Not quite. Despite a long lull that convinced even the most cautious Americans to return to “normal,” the virus continued to circulate — and evolve. Now, due to new variants and the natural ebbing of immunity, it’s starting to spread more widely.
More coverage of COVID on Yahoo News
The good news is that almost everyone has some form of immune protection, and that’s enough to keep serious illness at bay. (The number of Americans hospitalized with COVID, though rising, is currently level with previous low points during the pandemic.) The risk of long COVID is also lower today than ever before.
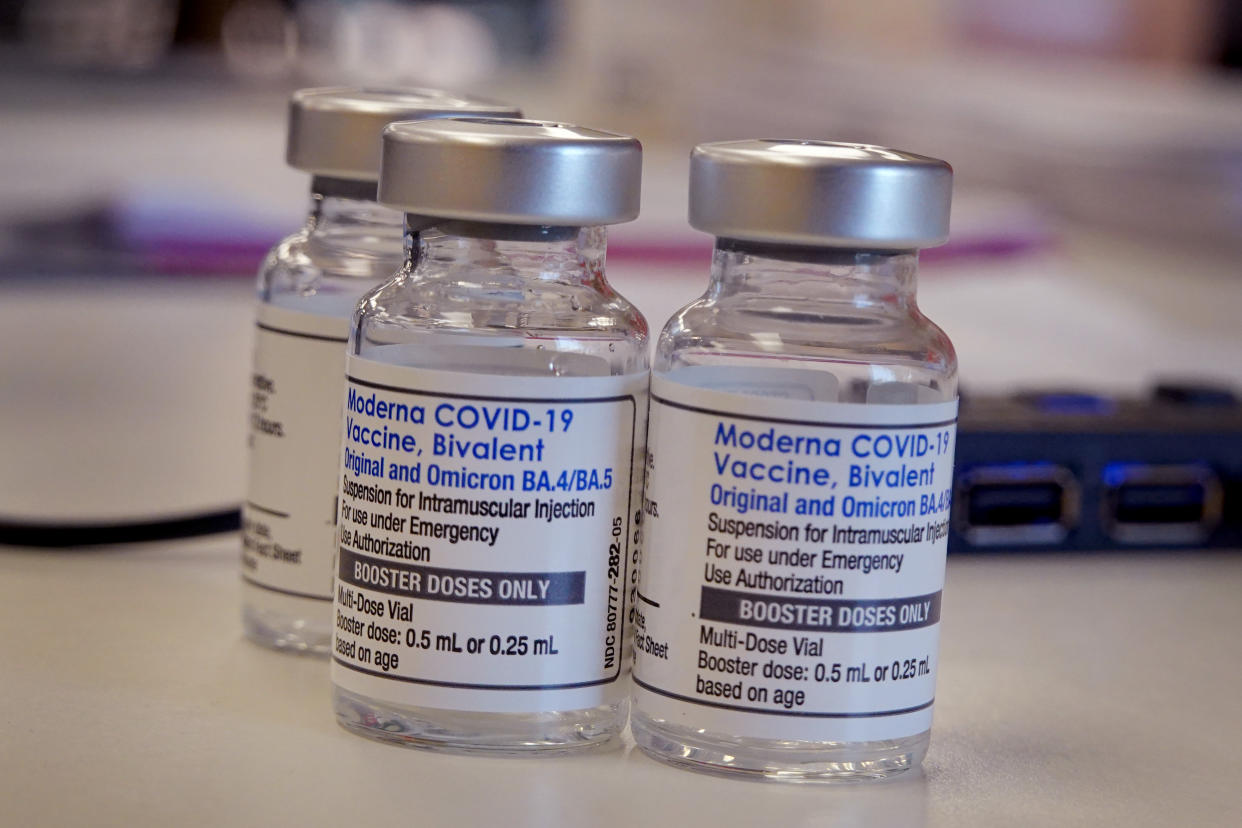
And new booster shots, expected in mid-September, will only bolster the body’s defenses.
So if the threat of COVID has largely receded — and if these sorts of waves will keep coming for the foreseeable future — do we still need to rearrange our lives when they do? Or can we finally treat COVID the way we treat other bugs like the flu?
Why am I suddenly hearing so much about COVID again?
Experts agree that three forces are likely at work. One is behavior; the more we return to normal, the more opportunities viruses have to spread. Another is waning immunity. It’s been a year since Americans got their last booster shots, and many haven’t had COVID since 2020 or 2021.
But probably the biggest factor behind the current wave is new variants. The most prevalent among them is EG.5 (nickname: Eris). Eris has one notable mutation that helps it evade antibodies, which probably explains how it became dominant worldwide. But the variant doesn’t have any new capacities in terms of contagiousness, symptoms or severity, so the World Health Organization says that “the public health risk posed by EG.5 is evaluated as low at the global level.”
Far less prevalent — but potentially more irksome — is BA.2.86 (nickname: Pirola). Unlike Eris, Pirola boasts so many mutations (about 35) that it represents “an evolutionary jump similar in size” to the first Omicron variant, according to virologist Jesse Bloom of the Fred Hutchinson Cancer Center.
Initially, researchers feared that vaccines and previous infections wouldn’t do much to shield people from Pirola. But three studies released this week show that “the variant does not penetrate cells very well” and that it doesn’t evade the immune system as much as expected.
New data out Tuesday from Moderna found that its updated booster generated a nearly ninefold increase in neutralizing antibodies against Pirola — meaning that the forthcoming shots will likely remain effective.
As a result, Pirola has “been downgraded from a hurricane to not even a tropical storm,” Eric Topol of Scripps Research told USA Today.
What about long COVID?
For many people, the fear of hospitalization or death from COVID subsided long ago. But they remain cautious because they’ve read that some infections trigger long-term symptoms such as brain fog and crushing fatigue — aka long COVID.
Yet long COVID, while real, is a lot less common and persistent than initially reported. In fact, now that immunity is widespread, it’s probably not that much different from the kind of rare post-viral illnesses that occasionally follow other respiratory infections.
A 2022 Israeli study of 150,000 patients, for instance, found that just 407 of those who had COVID also reported having persistent concentration and memory problems one year later — only slightly more than in the control group.
Read more from Yahoo News:No, you don’t have the flu already. It’s probably COVID, via Insider
Likewise, a 2022 British study of more than a million patients “found no evidence of a greater overall risk of any first neurological or psychiatric diagnosis after COVID-19 than after any other respiratory infection.” And researchers at Montefiore Medical Center in New York City recently discovered that just 2% of their COVID patients reported new-onset neuropsychiatric symptoms — versus 2.5% of their flu patients.
Overall, the share of COVID-19 patients who currently say they have long COVID fell by 42% between June 2022 and January 2023, according to the U.S. Census Bureau. Studies also show that vaccination lowers the risk of long-term symptoms, as does Paxlovid.
In short, the idea that COVID is uniquely likely to result in serious symptoms that last for more than a year is becoming less true all the time.
So do I still have to treat COVID differently than other viruses?
The era of mask mandates and vaccine requirements has long since ended. So personal risk tolerance and responsibility has been (and will continue to be) key. If you don’t want to catch COVID or pass it to someone else, you know what to do: Vaccinate, mask, test and isolate if positive.
For now, COVID remains riskier than influenza; a report published in JAMA in April found that COVID still killed hospitalized patients nearly twice as often as the flu. But those numbers are on track to become roughly equivalent over the next year or so, to the point where bothviruses may be responsible for fewer than 50,000 annual U.S. deaths.
Until then, additional caution is warranted for (and around) higher-risk individuals, such as seniors. President Biden struck this sort of balance when he tested and masked after his wife contracted the virus — but kept his plans after testing negative himself.
Longer term, the smartest and most sustainable approach may be to stop treating COVID as an exceptional threat, while also recognizing that our choices affect those around us.
“When you are sick, don’t soldier through it; rest, and try not to spread it,” Slate’s Shannon Palus recently explained. “It doesn’t have to change your whole life. But with a little attention, what we went through with COVID might apply, just a little bit, to everything else.”


