Professor Alasdair Geddes, infectious disease expert who diagnosed the last case of smallpox – obituary

Professor Alasdair Geddes, who has died aged 89, was an expert in infectious diseases who diagnosed smallpox in the last recorded person to die of the disease anywhere in the world; later, following the September 11 attacks, he became an adviser on bioterrorism for the Department of Health.
In August 1978, after successful vaccination campaigns and after what was widely thought to have been the last ever case of smallpox, in 1977 in Somalia, the World Health Organisation (WHO) was gearing up to announce the wordwide eradication of the lethal virus.
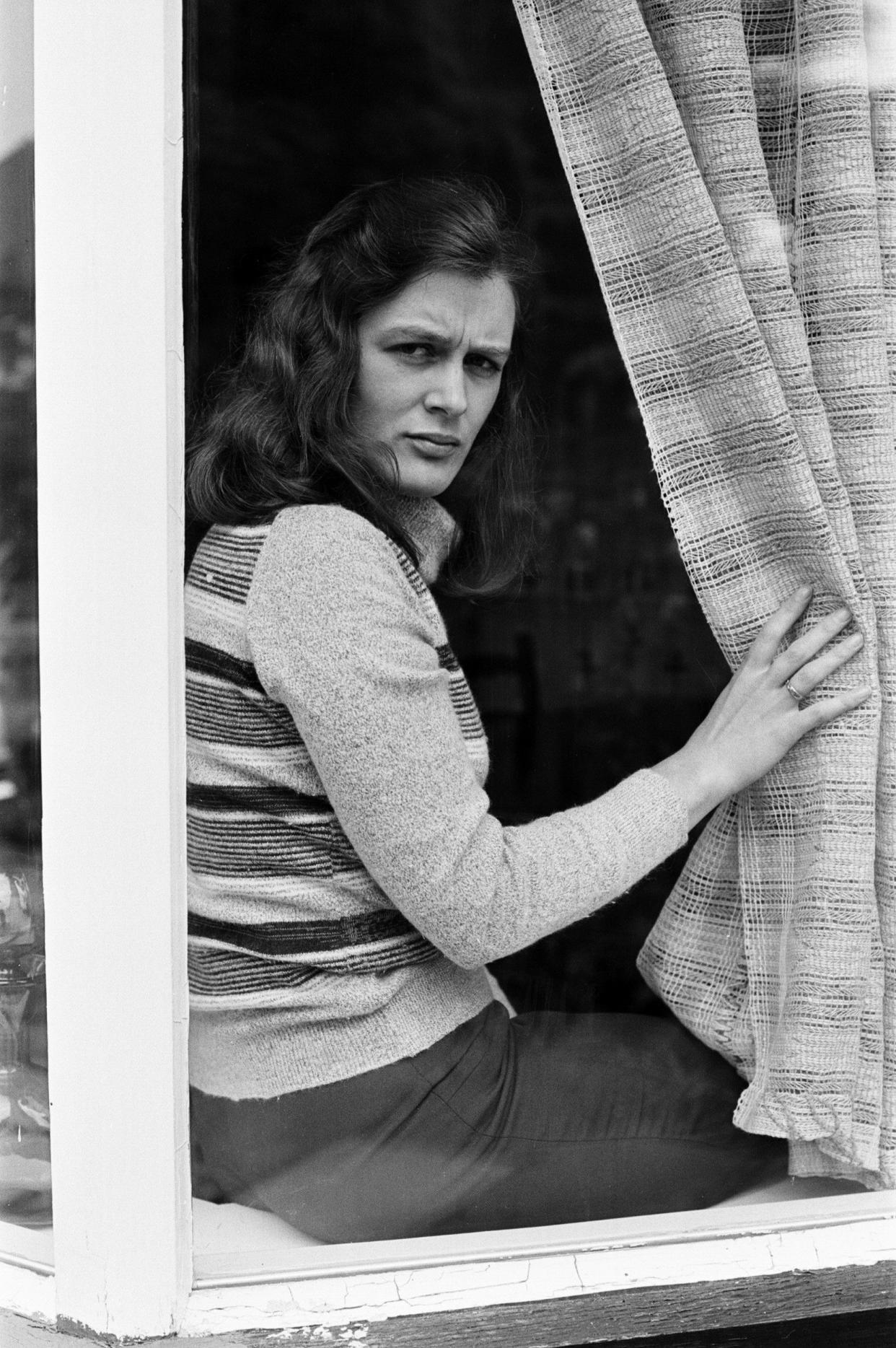
On August 11 1978, however, Janet Parker, a 40-year-old photographer at the University of Birmingham medical school, went home from work with a splitting headache. By August 16 she had developed a rash on her chest, limbs and face. Her GP made a tentative diagnosis of chickenpox, though she had had the illness as a child.
At 3 pm on August 20 she was admitted to East Birmingham Hospital. She had a temperature of 38C, complained of aching limbs, and had pustules all over her body. Physicians who examined her initially were perplexed. As the last known case of smallpox had been announced the previous year, the disease was the last thing on their minds. Geddes was called in for an opinion.
Arriving at her bedside at 8pm, he immediately suspected smallpox. He was aware that Janet Parker’s darkroom was above a laboratory at the medical school that, under its director Professor Henry Bedson, an internationally recognised expert on smallpox, was one of only a handful commissioned by the WHO to research the virus. Bedson and his team had been conducting research on variants known as “whitepox viruses”, which were thought to be a threat to the WHO’s eradication programme.
Geddes immediately rang Bedson, saying: “I have a suspected smallpox here, Henry, and it’s a lady who works as a photographer in the medical school.” Geddes took fluid samples from her blisters and drove to the medical school, where he met Bedson.
At about 10pm Bedson put the samples into an electron microscope. “I said ‘can you see anything Henry?’,” Geddes recalled, “and he never answered. So I gently moved his head aside so I could look down the microscope and there were brick-shaped particles that are characteristics of the smallpox virus. [Bedson] was horrified, because there was little doubt that in some way the smallpox virus had escaped from his laboratory and had infected Mrs Parker.”
The response of health and local authorities in Birmingham, backed up by a team of experts from the WHO, was remarkable. By the time Geddes’s diagnosis was confirmed, Janet Parker was on her way to an isolation hospital near Solihull. By 11 pm all her close contacts, including her parents, had been placed in quarantine.
Within 24 hours, most other recent contacts – family, friends, colleagues, neighbours, GPs who saw her before she got to hospital, and hospital staff, were in quarantine. Anyone who had visited the infectious diseases unit on the day she was admitted, or had been near her home (refuse collectors, people delivering newspapers and milk and so on) were placed under surveillance.
“It was huge,” Geddes, recalled. “Smallpox was about to be declared eradicated, people knew that was about to happen, it was a feared disease; it wasn’t just a panic in Birmingham, there was panic in the government and the WHO of it just reappearing. Very very quickly, national and then international press appeared and it became a major worldwide issue.”
Janet Parker died on September 11 1978. Due to the risk of infection, no post mortem examination was carried out and her body had to be cremated due to fears that the virus might have lived on in the ground if she had been buried.
But she was not the first victim of the outbreak. On September 5, Janet’s 71-year-old father Frederick, believed to be clear of the virus, died of a heart attack while in quarantine, thought to have been brought on by the stress of his daughter’s illness. The following day Bedson, who had been left “distraught” by the outbreak, cut his throat in his garden shed, his obituary in the British Medical Journal reporting that his “normally stable personality” had broken down after “journalists launched a relentless effort to fix the blame [for the outbreak] on him”.
As Geddes recalled, “The incubation period for smallpox is quite long, it’s about 12 days, so we had really about a fortnight’s anxiety to whether there were going to be any more cases.” Janet’s mother was diagnosed with the disease, but survived. As the result of measures taken to contain the outbreak she was the only other person infected; Birmingham was officially declared free of smallpox on October 16.
Although it was clear that the virus had originated in the smallpox lab, exactly how Janet Parker came to be contaminated remains a mystery to this day. A government-commissioned paper suggested that the virus had probably travelled in air currents up a service duct from the laboratory via an enclosed courtyard to the photography department on the first floor, but that idea was rejected during a 1979 court action by the Health and Safety Executive against the University of Birmingham for breach of safety laws.
Experts found there was not enough of the virus produced at the lab to cause death in the room above. Moreover while the government enquiry noted the poor state of duct sealing in the laboratory, this had been caused after the outbreak by engineers fumigating the laboratory. The university was found not guilty.
Geddes’s memories of 1978 inspired Mark Pallen to write The Last Days of Smallpox: Tragedy in Birmingham, published in 2018.
Alasdair Macintosh Geddes was born on May 14 1934 at Fortrose, near Inverness, to Angus and Isabella Geddes. From Fortrose Academy, he studied medicine at the University of Edinburgh and worked at the Royal Infirmary in Edinburgh and then in Perth, before National Service in the RAMC.
He began specialising in infectious diseases at Edinburgh and then as a medical registrar at Aberdeen where he researched antibiotics. In 1967 he took up a post as a consultant in infectious diseases at the East Birmingham (now Heartlands) Hospital.
In 1973 he spent seven weeks as a visiting fellow with the WHO smallpox eradication effort in Bangladesh, where he saw many cases of the disease. The following year, in an article in the BMJ he warned that the possibility of smallpox should be considered in every patient with unexplained fever who had recently visited India, Pakistan, Bangladesh, Nepal or Ethiopia, where the disease was then still endemic.
Geddes was appointed professor of infectious diseases at Birmingham University in 1982. In 1991 he was appointed professor of infection at the university’s medical school, where he served as Deputy Dean then Associate Dean.
In the 1990s Geddes became involved in studying the molecular biology of the TB bacterium Mycobacterium tuberculosis, researching new ways of delivering medicines into TB infected cells.
Geddes served widely as a consultant, and member or chairman of bodies concerned with infectious diseases and medicine safety. The author of some 200 scientific papers, he served as chairman of the first editorial board of the Journal of Antimicrobial Chemotherapy, as editor-in-chief of the International Journal of Antimicrobial Agents and co-edited the best-selling Control of Hospital Infection (now known as Ayliffe’s Control of Healthcare-Associated Infection: A Practical Handbook). From 1996 to 1998 he was president of the International Society for Infectious Diseases.
As a government adviser on bioterrorism after the September 11 attacks he emphasised the need to train physicians to diagnose disease caused by biological agents including smallpox as part of national preparedness plans. In 2006 he published The History of Smallpox.
Geddes recalled that when he first told his medical friends in Edinburgh that he was going to work in infectious diseases, “They said you’re mad, infectious diseases are disappearing, we have antibiotics and vaccines, why don’t you do something more interesting?”
But, as he observed in 1995, “Nature will never allow a microbiological vacuum. It is a natural trend for new diseases to appear and for old ones to re-emerge. Tuberculosis, for example, which everyone thought was disappearing, has re-surfaced... And if the world experiences global warming, as the scientists predict, we in this country could have to deal with tropical diseases, such as malaria.”
The recipient of numerous awards, Geddes was appointed CBE in 1996.
He is survived by his wife Angela and by two sons.
Professor Alasdair Geddes, born May 14 1934, died April 9 2024


