How Jersey is on the brink of assisted dying – and Scotland could be next

One hundred miles from mainland Britain – a good deal closer to Saint Malo than to Salcombe – Jersey should really feel more French than British.Its street names are Gallic but the island looks and feels like a sleepy stretch of the south coast.
Victor Hugo once described it as a piece of France “fallen into the sea and picked up by England”. In fact, it’s neither. It isn’t part of the United Kingdom, it’s a Crown Dependency, autonomous and self-governing. And yet, to those of us living on mainland Britain, it’s as British as Anglesey, Lindisfarne or Orkney.
So, as Jersey prepares to vote through a law that would allow people to legally end their lives on the island, those 100 miles have never seemed shorter.
Jersey is set to become a canary in the coalmine for Britain on assisted dying. On Friday, the government published proposals for what the legislation could look like.
They outline what some consider to be sensible parameters, while for others, the proposals represent a slippery slope which could one day lead to a model like that in the Netherlands, where people with a history of depression or anorexia have chosen to legally end their lives.
The proposals state that to be eligible you will have to have lived on the island for 12 months (a stipulation that it said was “intended to discourage ‘death tourism’”). There are two possible routes to assisted dying laid out. In the first, you would have to be terminally ill, with a prognosis of six months for cancer or 12 months for a neurodegenerative condition like Motor Neurone Disease.
Route two would allow for someone with an incurable physical condition, which causes unbearable suffering which “cannot be alleviated in a manner the person deems to be tolerable”, to be eligible. Someone who had been paralysed below the neck, experienced chronic pain and needed 24 hour care, for example, would be eligible under route two.
In both cases, you must possess the capacity to make the decision.
A nine-week lodging period will now follow; a debate on the proposals is scheduled for May 21. If voted through, it’s expected it could take 18 months to draft a law. The earliest it could come into effect would be spring 2027, but however long the process takes, it is looking likely that assisted dying will become a reality on Jersey.
It’s a watershed moment for Britain, coming amid growing pressure in the UK with public figures like Esther Rantzen – who revealed in December she was considering assisted dying – calling for a change.
Sir Keir Starmer has pledged parliament will debate and vote on assisted dying if Labour wins the next election. Meanwhile, Jersey isn’t the only jurisdiction on the cusp of making such a move.
The Isle of Man has a bill at committee stage having backed a proposal in October to allow terminally ill people to choose an assisted death. In the Scottish parliament, it was announced this week that a private member’s bill would be considered.
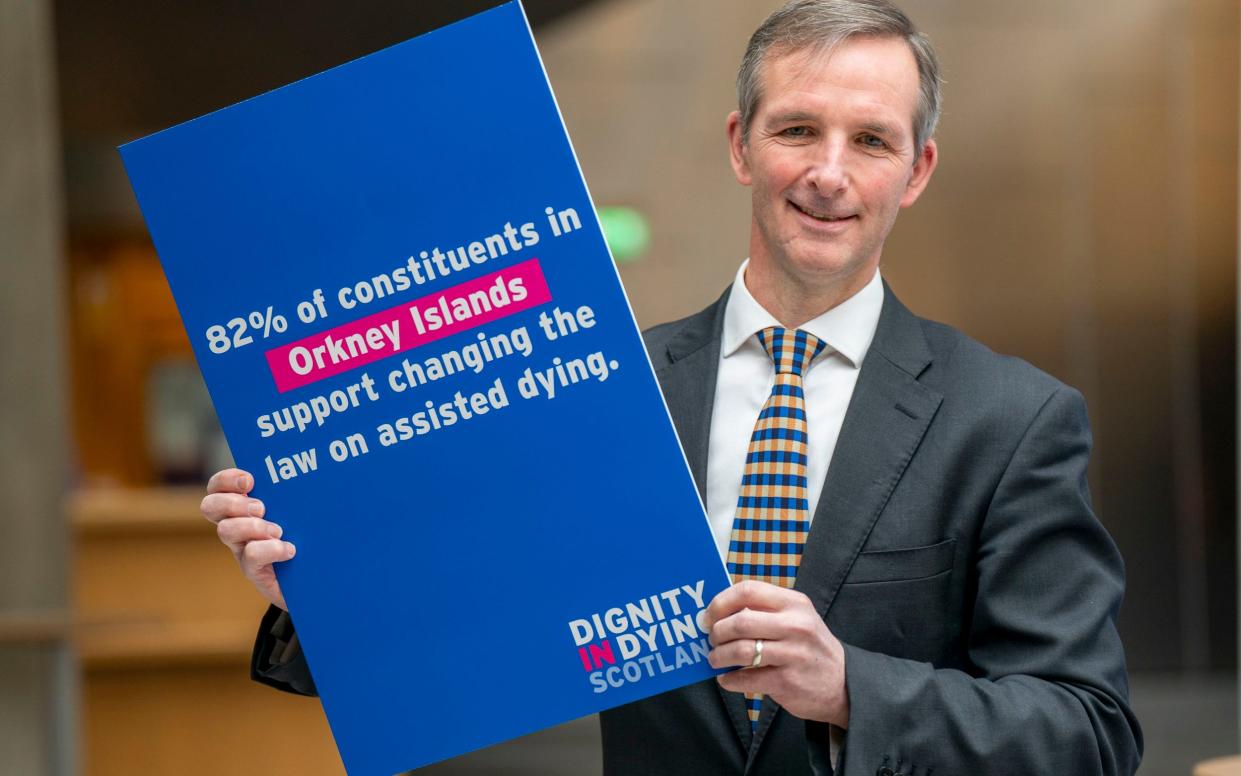
Liam McArthur, Lib Dem MSP for Orkney, wants to pass the Assisted Dying Bill in 2025. If voted through, it would make Scotland the first UK nation to legalise assisted dying.
Last month, a report from the health and social care committee warned MPs to consider the repercussions of a law change anywhere in the British Isles. “Ministers should be actively involved in discussions about how to approach the divergence in legislation.”
On Jersey, the debate has divided the island. A citizens’ jury convened in 2021 agreed overwhelmingly that, if subject to “stringent safeguards”, assisted dying should be permitted. 78 per cent of the jury were in favour, but campaigners against assisted dying – including healthcare professionals who would be forced to become conscientious objectors if the law went through – say it is both deeply wrong and could be catastrophic for the island’s healthcare system.
Behind the debate on Jersey are people with terminal diagnoses desperately hoping the law will be enacted in time for them to use it. Then there are people for whom the concept of state sanctioned suicide is ethically wrong – people who feel even the strictest legislation would be the beginning of a road no society should ever venture down.
Lorna Pirozzolo is in the first camp. She was diagnosed with stage four terminal breast cancer in 2019. Five years would have been a “realistic” prognosis then; she has exceeded that by two months and counting, though not without bumps in the road.
Initially, Pirozzolo, in her 40s, who works in air traffic control at Jersey Airport, tried “to stay out of the debate” on assisted dying. Then, in late 2019, she began experiencing a pain so bad it made her confront the realities of what “unbearable suffering” (which the legislation would require people to prove) might genuinely feel like.
For months she would be rushed to hospital with recurrent pancreatitis. The pain was so bad it made her black out. At its worst, it was happening twice a week. Once, doctors had to put her in a coma to stop the pain. “They say you can’t define unbearable pain. You can. Neither your body nor your mind can go on like that. So of course I begged a nurse to kill me.”
A low winter sun is setting over the island as we talk in the cosy living room of her in-laws’ home. Pirozzolo and her husband, Joe, a business consultant, are living here while they do up a house nearby. It is a week before the proposals are to be published and Pirozzolo has had “a really bad fortnight”.
Her pancreatitis has calmed down thanks to surgery in 2022 to remove her gallbladder, but the drugs she takes are gruelling. Any time she feels a new sensation – a headache, an itch, anything out of the ordinary, she knows it could be a sign the cancer has once again metastasised.
There is no clear roadmap for what the end of her illness might look like, but she knows she doesn’t want to experience anything like the pain she felt during those terrible months, when she went as far as to “pick a date” to die. “[It] was going to be November 11, three weeks after surgery.

“We’d know by then if it had worked. I was going to have to take my own life. It wasn’t a choice. I’m not saying I wanted to kill myself – I didn’t have a choice in that. It was like, if surgery doesn’t work, you just can’t…”
Thankfully, it worked. But afterwards, Pirozzolo began “proactively contacting politicians about assisted dying”. She realised that if her surgery had failed, she would have been forced “to die on my own”.
If Pirozzolo didn’t mention she was currently in the midst of a bad patch, you would never know – she seems full of energy. She is sharp and fiercely bright. You don’t have to spend much time with her to see she is made of steel. Her pet hate is when cancer patients are labelled “vulnerable”.
Pirozzolo is very clear that she doesn’t want to die, but she’s realistic about what the end could be like. “I’m not scared of death itself,” she says. “It’s the bit before it. What you’re going to be made to go through.
“It’s not that you want to die – you don’t want to leave your loved ones. [...] But I don’t want to be in excruciating pain and forced to stay in it.”
Some argue end of life care is so advanced now that it should be possible to have a “good death”. “If you’re saying people can be rendered unconscious then I agree,” says Pirozzolo, “but to me, unconscious is not acceptable”.
A strong argument against assisted dying is the risk that people (especially the elderly) could be put under pressure to die. Pirozzolo points out that many cancer patients feel under pressure “to take the next medicine no matter what it puts our body through”. “Do they ever stop to think when they’re putting us under pressure to keep living?”
She had a “polite” debate recently with a religious man on the island who was arguing on the opposite side of the debate. By the time he had heard Pirozzolo’s story, he seemed to have relented a little: “[He said]: ‘I have to admit I have never experienced that kind of pain. [...] If you were in that much pain, come the end of your life because of cancer, I can understand that.’ And I’m thinking, well, that’s what we’re fighting for.”
With others in the community, she simply avoids the topic, as with one man who she knows opposes the legislation. “I’ve bumped into him a couple of times and we just don’t discuss this.”
For many on Jersey, the proposals are deeply worrying. Andreas Melchior, a practising GP on the island, fears where the proposals could lead. “I understand that people want the choice,” he says. “But this is crossing a line that we have to be very careful of because you can’t go back over that line. [Assisted dying] has had a lot of unintended consequences in all the jurisdictions where it’s been done.”

In countries like Canada and Holland, he says, where assisted dying is legal, the law has gradually expanded. “Within a very short space of time, the legal challenges came, the safeguards were removed, and they’re now euthanising a lot of people that were never planned to be included in this proposal. We worry it’ll happen the same on Jersey.”
We meet at the house of a GP friend of Melchior’s, John Stewart-Jones. Now retired, Stewart-Jones feels assisted dying goes against the Hippocratic Oath he made when he first qualified. “When you’ve given your life to care for people and do the best for them, to actually go and kill them is completely contrary to most doctors’ conscience.”
Both worry about the impact the legislation could have on the island’s health system. “In Jersey we don’t have enough GPs, we don’t have enough palliative care people, we don’t have enough mental health doctors,” says Melchior. “If we draw off some of those people in order to make assessments for people being processed for dying, that would deprive the healthcare system of professionals.”
They aren’t convinced enough doctors would want to participate. “A lot of health professionals on this island, when you ask them privately, they say I don’t want anything to do with it.”
One GP who would be prepared is Nigel Minihane. For him, the slippery slope argument doesn’t hold up. “You can make your legislation quite definitive,” he says. “And we’ve done that with abortion. Abortion legislation hasn’t changed for 60 years.”

Limiting the legislation is crucial, he says. For Minihane, a patient should be “actively dying”, or “the safeguarding issues are far, far too great”. He is more in favour of route one than route two, for which he fears “there would have to be many more tribunals and legal processes”.
Jersey’s healthcare system is no more robust than our own NHS. “Our health system is failing like your health system,” he says. “It doesn’t have the money to do what it needs to do anyway, and I would hate to see resources being devoted to lawyers at the expense of the health system.”
With route one, however, the risk is lower, the numbers more predictable. “We know there are a certain number of people actively dying every year who will fall in the category and only very few of those will come into the category where they’d want to take their own lives.”
Doctors and campaigners are divided on a crucial point: the effectiveness of end of life care. Melchior and Stewart-Jones are among those who say it is possible to have a good death, that the right drugs can make someone comfortable. Minihane says otherwise. “Palliative care is not a panacea. People assume it is – that if palliative care were better everything would be perfect. [...] I have seen bad deaths and bad deaths continue to occur.”

They might be “rare”, he says, but “sometimes pain can’t be managed because it’s so severe”. “Some people would argue you can knock people out. [...] But how long do you sedate them for? Ethically, what’s the difference between sedating people to the point of unconsciousness until they die as opposed to them making a decision where they die?”
If it were to happen, opinions are split on whether there should be a Dignitas-style clinic, or a service folded into healthcare like palliative treatment, with people dying in hospices, hospitals and at home. Stewart-Jones is opposed to either, but feels the first option would be “the lesser evil of the two”. For Minihane, the “where” shouldn’t be so prescriptive. “It’s back to choice”. “People die in hospice, in hospitals, at home. Why would this be different?”
Politicians on the island are split on the matter. Jennifer Bridge MBE, a former States Member, says Jersey is well set up to enact this legislation. “The fact that we’ve got a functioning health service and an absolutely superb hospice means that there’s a framework where this can sit,” she says.

Others have spoken out about the possible risk to vulnerable people. “Safeguards can be built up and to the best of our ability, but none of them can be truly effective,” said Minister for Health and Social Services, Richard Renouf, during a debate on the issue in 2021.
“None of them would truly protect patients who are going to become vulnerable if assisted dying were to be introduced.”
Some have actively put aside personal beliefs. “I would never want anyone to restrict my choices on something that impacts me and my body,” Deputy Carina Alves said in 2021, when the principle of assisted dying was first approved. “Regardless of my faith, I have no right to do that.”
Faith is a factor for many in the anti-assisted dying campaign on Jersey. Stewart-Jones and Melchior met when they attended the same church on the island, though both say faith is only part of the story for them. It’s “my professional view and my ethical view”, says Melchior.
Sarah Whooton, Chief Executive of Dignity in Dying, said Friday’s proposals should prompt MPs in Westminster to “take note”. “Assisted dying is firmly on the electorate’s agenda as we approach what is set to be a watershed General Election.” The charity’s latest polling, carried out by Opinium, showed 75 per cent of Brits support assisted dying.
For Pirozzolo, a change in the law on Jersey can’t come soon enough. She wouldn’t consider going to Dignitas – the £15,000 price tag would be a stretch. She is getting her affairs in order – she’s nearly paid off her funeral, and is in the process of choosing the music. Sunshine on Leith, she thinks.
If she could choose how her last day would go, what would it look like? She suspects it’ll be in the island’s “beautiful” hospice. But given the choice, she’d go down to the beach with her husband and her twin sister. “You take something and then you just go down to the lighthouse listening to the waves.”
“Whether that will be allowed legally, I don’t know. But that would be my ideal.”


