Covid-19 patients on ventilators at highest level for more than two months
The number of Covid-19 patients on ventilators in England’s hospitals has climbed to its highest level for more than two months, new figures show.
Analysis by the PA news agency shows that the average number of patients in hospitals in England is also climbing, with younger people driving the rise.
The average number of patients with Covid-19 in England in mechanical ventilation beds stood at 245 on June 29, according to the NHS England figures.
This is up from 206 a week earlier and is the highest since April 24, having dipped as low as 113 on May 29.
The number is still far below the peak of the second wave, when the average hit a high of 3,676 on January 26.
But the trend suggests there is still enough of a link between Covid-19 infection and hospital admissions to result in a growing number of people needing intensive treatment.
The data for England also shows that the total number of hospital patients with Covid-19 is currently averaging 1,333, the highest number for exactly two months.
At the peak of the second wave, patient numbers reached an average of 33,594.
For the UK as a whole, the average number of Covid-19 patients stood at 1,525 on June 27, the highest since April 30.
And the daily average for UK hospital admissions stood at 229 on June 23, the highest since April 6.
People aged 18 to 64 are driving the increase in admissions and are the group most likely to have had just one vaccine or no vaccine.
As of June 27, hospital admissions in England of people aged 85 and over are averaging just 12 a day, close to this year’s all-time low of seven a day, and far below the average for the peak of the second wave (789).
Admissions for those aged 65 to 84 have increased slightly in recent weeks and are currently averaging 42 a day, compared with a low of 16 in late May – though this is also well below the second-wave peak (1,578).
Meanwhile, for those aged 18 to 64, daily admissions are currently averaging 133.
This is the highest number for three months, up from a low of 42 in mid-May.
These numbers are still some way from a second-wave peak of 1,403, but represent a clear upwards trend.
Downing Street said that the NHS was prepared for an increase in admissions of coronavirus patients to intensive care.
The Prime Minister’s official spokesman said the rise had been anticipated and the country remained in a “good position” to continue with the lifting of lockdown restrictions on July 19.
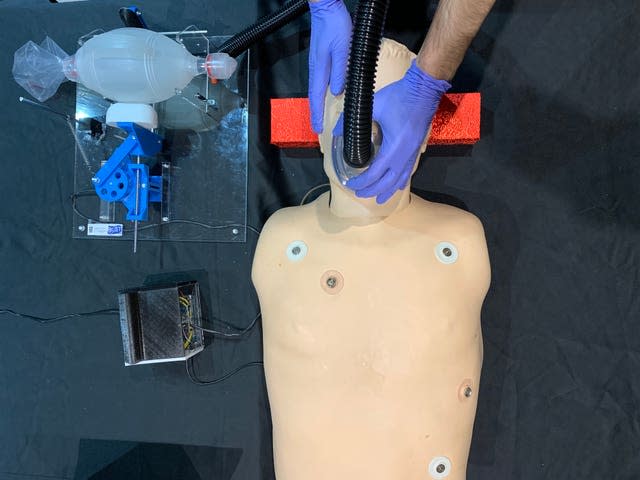
“We have put in a number of additional measures, not least additional ventilators, so we are prepared for this,” the spokesman said.
“As we have said all along, we know cases will rise, sadly we know that will lead to an increase in hospitalisations and whilst the increase has not been as significant as in the past we have seen numbers increase.

“We are aware of the huge challenge this pandemic continues to pose to the country but it is thanks to the significant defences that we have built up through our vaccination programme that we have been able to be one of the most unlocked countries in Europe and in a good position still to take a further step later this month.”
It comes as Professor Stephen Reicher, from the University of St Andrews and a member of the Scientific Advisory Group for Emergencies (Sage) subcommittee on behavioural science, said the country was in danger of repeating last summer’s mistakes
In the warmer months last year, people enjoyed relative freedom before restrictions were reimposed heavily over the winter.
Prof Reicher told Times Radio: “My fear is that we’re on line to repeat the mistakes of last summer, if you remember, the Prime Minister told us it was our patriotic duty to go to the pub, that people should go to work or they might lose their jobs, we had eat out to help out.
“The consequence was we never got infections low enough to be able to deal with the disease and so when conditions changed in the autumn, when schools went back and people went back to work and universities went back and the weather got worse and we went inside, so infections spiked.
“And I think this time round, we should learn from that and we should get infections low to a point where we’re in a much better place in the autumn, where we don’t have to reimpose restrictions.”

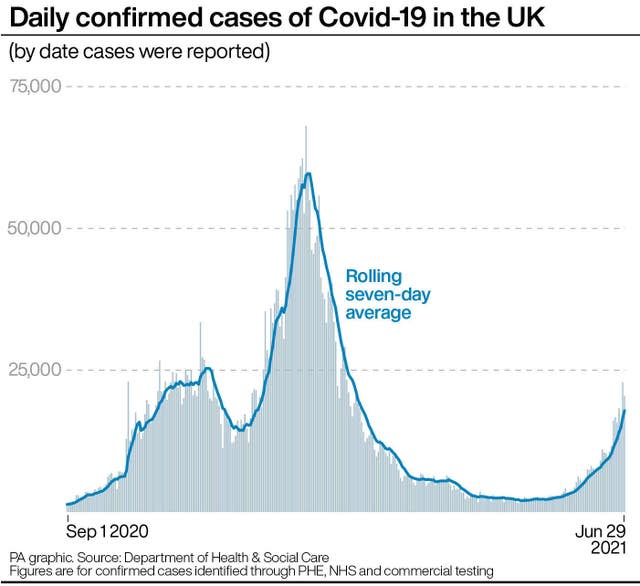
The latest daily figures show there were 20,479 new infections reported in the UK on Tuesday, and 23 deaths within 28 days of a positive test were recorded.
Prof Reicher said he believed vaccines had weakened the link between cases and hospital admissions but had not broken it.
He said that “vaccination has made a huge difference but the danger is if we overstate it, and we over-rely on it, actually we undermine all its good effects”.
He added: “So it’s belt and braces, of course vaccination makes a difference but it doesn’t mean you forget about everything else.”
He suggested there needed to be more support for people isolating, better ventilation and public health measures and a speeded-up test and trace system.


