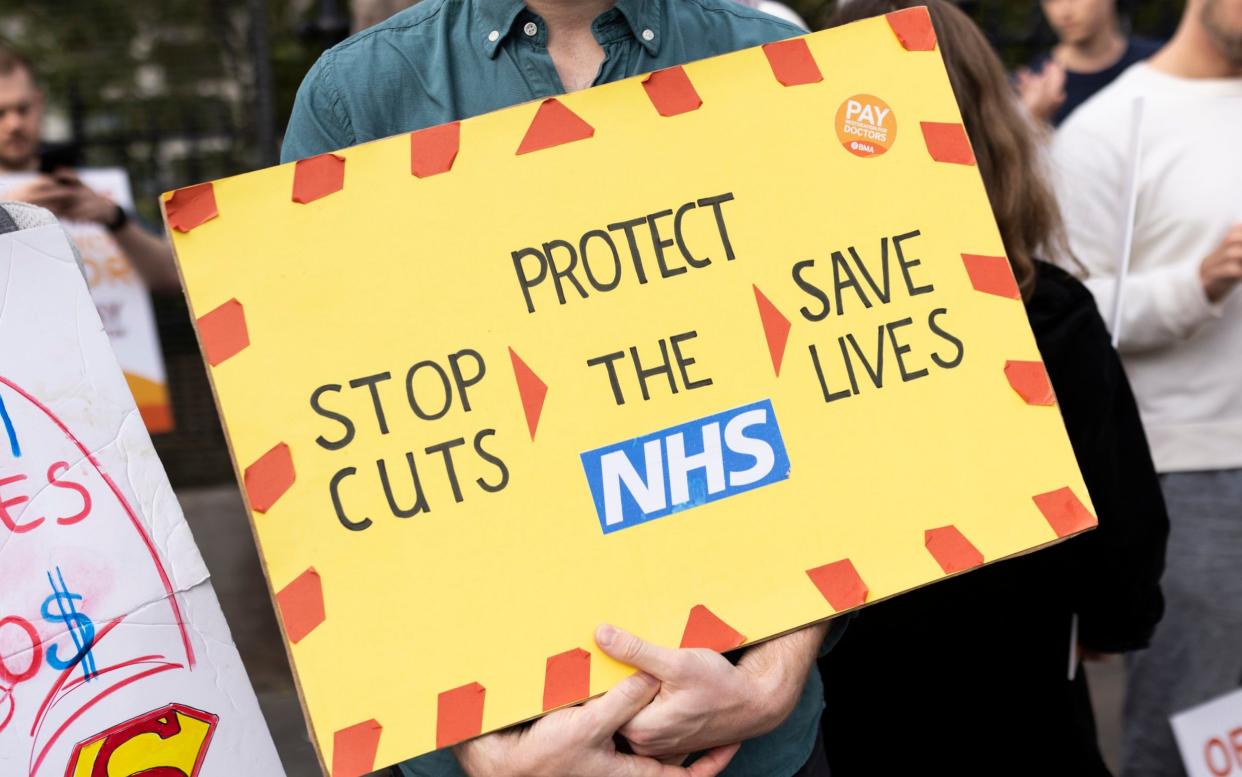
Record number of excess deaths amid NHS strikes

Britain experienced a record number of excess deaths last year amid repeated NHS strikes and the continued cost of the Covid pandemic.
Nearly 53,000 more people died in 2023 than normal – the highest figure recorded in a non-pandemic year since the Second World War, Telegraph analysis shows.
Doctors went on strike for 38 days last year, and experts fear the disruption contributed to the high number of excess deaths.
On Wednesday, junior doctors start the longest strike in the history of the health service. Officials have said the walkout will mean “the most difficult start to the year the NHS has ever faced”.
Prof Carl Heneghan, director of the Centre for Evidence-Based Medicine at University of Oxford, told the Telegraph that patients had been “abandoned to look after themselves” while doctors and the Government were “at a standoff”.
He said: “Patients are being rung up with diagnoses for cancer over the phone, left abandoned to look after themselves while the strikes are worked through, and it’s patients that are ultimately suffering.”
NHS medical director Professor Sir Stephen Powis said the next strike, lasting six days, will cause a “serious impact in the weeks after” as services try to recover and deal with extra demand.
Experts have also said that the impact of the pandemic, lockdowns, and the resulting long waiting lists have all contributed to excess deaths.
The British Medical Association (BMA), the doctors’ union, has also been warned by NHS chiefs that the patients at the greatest risk of harm this week, based on an analysis of previous strikes, were those with fast-progressing cancers, time-critical inductions and urgent “elective” C-sections, and corneal transplant surgery.
Analysis by The Telegraph of Office for National Statistics (ONS) figures for England, Wales and Scotland showed that 52,698 more deaths than would have been expected had occurred by Dec 8 last year, based on a five-year average of deaths before Covid.
Official ONS analysis to calculate the five-year average excludes 2020 but includes 2021, which was still heavily impacted by Covid. The total number of deaths last year was 595,789.
It means there were more than 1,000 additional deaths each week, surpassing last year’s total of 50,200 and the peak of 51,200 during the 1951 flu epidemic. It is the highest figure since 1940, before the NHS existed, when there were about 96,000 extra deaths.
During the pandemic, 82,000 and 60,000 extra deaths occurred in 2020 and 2021, respectively.
Prof Heneghan said: “We’re at a tipping point in the NHS. People are dying on the waiting list, those who require emergency care are not being sought and seen quickly enough, and social care is almost non-existent.”
He said many GPs had not worked for seven of the last 10 days, with a quarter of their number being made up of junior doctors.
Prof Heneghan said cancer patients normally seen in a clinic and starting treatment were being called by overstretched consultants instead of seen in person, and everything was being pushed back because of strikes.
“Consultants are covering the junior doctors’ work and so there is a displacement and basic care is going out of the window,” he added. “I would implore at this time of year that both sides need to just get around the table and call this strike off.
“Both sides seem to be at a standoff where they’re almost holding a gun to each other’s head. This should now be a job for the Prime Minister to act, because it is patients that will suffer – and suffer in many different ways. It is completely unacceptable to play with people’s lives in this way.”
Dr Tim Cooksley, a former president of the Society of Acute Medicine, said the strikes “reflect the stress and pressure and frustration that [staff] can’t deliver the care they want”. He added: “Industrial action increases pressure on services, and this can lead to adverse effects and harm for patients.”
Prof Karol Sikora, a leading cancer specialist, warned that Britain is still seeing a knock-on impact from Covid, adding: “A tunnel vision focus on one virus led to millions and millions of patients suffering delays in diagnosis and treatment for every single aspect of healthcare.
“Lockdowns, and the associated delays, are undoubtedly the driving factor behind these horrific statistics. In cancer alone, I estimate that there will be significantly more life years lost to unnecessary delays than the virus sadly took.”
Dr Adrian Boyle, the president of the Royal College of Emergency Medicine, said it was “vital” to remember that each death “represents an individual person with a family and loved ones” and that it was “heartbreaking to think that any one could have been avoided”.
“The NHS has had to deal with a series of significant challenges in the past 12 months. Last winter was the most difficult the service has ever experienced,” he added, citing “excessively long waits” across all services, with “all of this in addition to a series of strikes”.
He said: “We cannot definitively say that all – or any – of these issues have contributed to the rise in excess deaths, but what they do reflect is a health system that is not functioning properly. Increasingly, it is the whole system that is in need of intensive care to ensure this shocking figure does not rise again next year.”
Britain’s excess mortality was worse than any other developed country as of mid-October 2023, when comparable international data was available.
The death rate of 8.6 per cent above the expected amount for the year significantly outpaced Israel, the next worst country, with 5.5 per cent.
Excess deaths in Britain were around four times higher than Germany’s 2.2 per cent. New Zealand had 1.4 per cent more deaths than normal, while France had 1.7 per cent fewer than expected, a separate Telegraph analysis of the World Mortality Dataset revealed.
Data for Australia and the United States was only available up until mid-August, when excess deaths were at 8.4 per cent and 1.4 per cent, respectively. The UK’s figure at that time was 9.0 per cent.
Junior doctors have been asking for a 35 per cent pay rise since they first walked out last March. The NHS backlog has continued to grow since, rising to a high of 7.8 million before dropping slightly last month.
Data from the Office for Health Disparities shows that excess deaths are disproportionately affecting middle-aged people between 50 and 64, where they are 13.5 per cent higher than expected, as well as the under-25s – 11.8 per cent higher.
The data also show people dying more often than they should from cardiac and heart-related issues, respiratory infections and diabetes, among other conditions.
Excess deaths from heart failure are up 16 per cent in the last year. Cardiac and respiratory care have been among the worst hit specialities by NHS delays.
Junior doctors are scheduled to walk out at 7am on Jan 3 and will not return to work until 7am on Jan 9.
Prof Powis said: “This January could be one of the most difficult starts to the year the NHS has ever faced.
“Six consecutive days of industrial action comes at one of our busiest periods,” he added. “Our colleagues across the health service are doing their very best for patients every day with extensive preparations in place, but there’s no doubt they are starting 2024 on the back foot – not only will action impact next week, it will continue to have a serious impact in the weeks after, as we recover services and deal with additional demand.”
A Department of Health and Social Care spokesman said: “We urge the BMA junior doctors’ committee to call off their strikes and come back to the negotiating table so we can find a fair and reasonable solution, and so we can all get back to focusing on patients and their care.
“We know how distressing it is for patients who have had appointments and procedures cancelled, and we have provided £800 million to ensure patients continue to receive the highest quality care this winter and ease pressure on hospitals impacted by industrial action.
“NHS staff are working hard to prioritise resources to protect emergency treatment, critical care, neonatal care, maternity, and trauma, and to ensure we prioritise patients who have waited the longest for elective care and cancer surgery.”
The BMA was contacted for comment.


