Oxford's coronavirus vaccine linked to bleeding disorder in rare cases

The University of Oxford-AstraZeneca coronavirus vaccine may trigger a bleeding disorder in rare cases, research suggests.
The jab was approved after a study demonstrated it is up to 90% effective at warding off COVID-19, the disease caused by the infection.
The UK's unprecedented vaccine rollout has been credited for its plummeting coronavirus death rate, with 72 fatalities within 28 days of a positive test being registered on 8 June – a 94.5% reduction from 8 January's 1,325 peak.
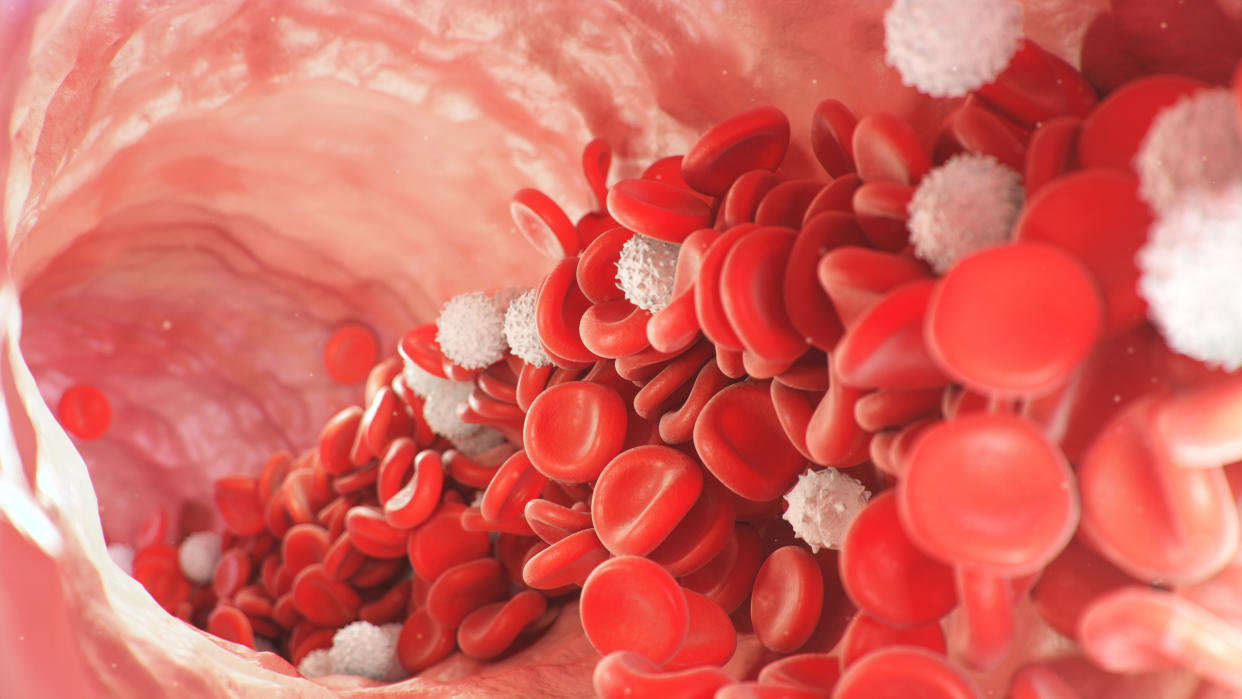
Although safe in the vast majority of cases, the Oxford-AstraZeneca vaccine has been linked to an unusual form of blood clots, defined by a low number of clotting cells called platelets.
Scientists from the University of Edinburgh have now reported that for every 100,000 first doses of the jab that are administered, around one case of idiopathic thrombocytopenic purpura (ITP) arises – a bleeding disorder caused by an insufficient number of platelets.
Read more: Man develops blood clot in his arm with asymptomatic coronavirus
While it may sound alarming, ITP is often mild, with a similar number of people developing the complication after a flu or measles, mumps and rubella (MMR) jab. Vaccines aside, around six cases are said to arise per 100,000 people "in the normal population".
The risk of developing ITP is also considerably higher with the coronavirus itself than any of its vaccines, with experts urging people to get immunised when called up.
"This careful analysis has found a small increase in the risk of ITP, clotting and bleeding events following the Oxford-AstraZeneca vaccine," said lead author Professor Aziz Sheikh.
"This very small risk is important, but needs to be seen within the context of the very clear benefits of the vaccines and potentially higher risks of these outcomes in those who develop COVID-19."
Platelets are released in response to a cut to prevent excessive bleeding.
Read more: Blood clot risk up to 10 times higher with coronavirus itself than its jabs
"ITP is a condition where the immune system destroys a person's own platelets," said Dr Will Lester, from the University Hospitals Birmingham NHS Foundation Trust.
"Bleeding symptoms are usually mild and death from ITP is very rare.
"In addition to bleeding, patients with ITP have a slightly higher risk of blood clots for reasons that are not completely understood."
The unusual clots that have been linked to the vaccine are thought to occur at a rate of 1.3 per 100,000 first doses. ITP is "likely to be a manifestation of this general condition".
The Edinburgh scientists analysed 5.4 people living in Scotland, of whom 2.5 million had received their first dose of the Oxford-AstraZeneca or Pfizer-BioNTech vaccine.
The UK has two others jabs in its immunisation arsenal against the pandemic – Moderna and the recently approved Janssen.
Up to 14 April, 1.7 million people in Scotland had received the first Oxford-AstraZeneca dose, while 800,000 had been immunised with the initial Pfizer-BioNTech jab. The scientists did not analyse the Janssen or Moderna vaccines, the latter of which was only recently rolled out.
The team combed through the 5.4 million participants' medical records, dating back to September 2019, to gauge whether any clotting or ITP events would have been expected to occur outside of the pandemic.
Read more: Mers a few mutations away from being a pandemic threat
Results – published in the journal Nature Medicine – suggest there was a "slight increase" in ITP events in the second week after an Oxford-AstraZeneca vaccine, as well as a "possible" rise in artery clots and general bleeding.
Unlike previous reports, the study did not link the jab to so-called cerebral venous sinus thrombosis (CVST), likely due to the very low number of participants who developed this side effect.
CVST occurs when a clot forms in the brain's venous sinuses, which prevents blood draining from the vital organ.
Watch: Do coronavirus vaccines affect fertility?
To put the ITP events into context, between one and three cases occur for every 100,000 vaccine doses administered against flu, MMR or hepatitis B.
"There is no evidence any specific type of vaccine for COVID is any more risky than any other or any more risky than other historical vaccines," said Dr Lester.
Professor Stephen Evans from the London School of Hygiene & Tropical Medicine agreed, adding: "This bleeding disorder occurs very frequently in COVID-19 itself, perhaps as much as 340 [cases] per 100,000 people getting the disease."
"Reassuringly", the Pfizer-BioNTech vaccine was not linked to ITP, clots or bleeding.
Read more: Long COVID patient unable to work a year after catching coronavirus
The study "adds to the evidence" the Oxford-AstraZeneca jab leads to clots and ITP in rare cases, but does not prove the vaccine directly causes these events.
"It is difficult to be certain whether these are vaccine-related or chance associations, although the close association of some to the vaccine suggests it is likely to be related," said Professor Adrian Newland, from Queen Mary University.
"To make matters rather more complicated, around one-third of adults with ITP are picked up incidentally and have no problems.
"We do not know in patients who present post-vaccine whether this was a new problem or highlighting an underlying disorder."
The UK's Medical and Healthcare products Regulatory Agency is said to be monitoring the situation.
Watch: What is long COVID?
"The good news is treatment [for ITP] is not always required and if it is, the [platelet] count usually responds quickly and is not associated with long-term disease," said Professor Newland.
In the Edinburgh study, the average age of the ITP patients was 69, with most having at least one underlying medical problem, like heart disease or diabetes.
Relatively few of the participants were under 40, as the Scottish vaccination programme prioritised the country's elderly residents.
Since the study was carried out, a decision was made to offer people under 40 a vaccine other than the Oxford-AstraZeneca jab, if possible.
Young people are thought to be more at risk of clots after the Oxford-AstraZeneca vaccine, but less likely to develop coronavirus complications themselves, skewing the jab's benefits relative to its risks.
"This study shows the advantage of being able to link together large national data sets to provide near real-time information of vaccine safety, using a number of analytical methods," said Professor Chris Robertson, from Public Health Scotland.
"An important next step is to replicate this work in other settings to ensure the findings are robust."



