What is the black fungus afflicting India's coronavirus patients?

India has become one of the worst-affected countries as the coronavirus pandemic continues to unfold.
After escaping the first wave relatively unscathed, the South Asian nation has recorded more than 25 million confirmed cases since the outbreak emerged – second only to the US.
Overcrowded living conditions, patchy healthcare and the emergence of a faster-spreading variant may have all contributed to the critical situation, with India setting a new global record for deaths in one day – 4,529 fatalities on 19 May, exceeding the US' 4,475 on 12 January.
While the pandemic is a worldwide issue, a so-called "black fungus" is disproportionately afflicting India's coronavirus patients.
Read more: What we know about India's coronavirus variant
As of April 2021, 41 coronavirus-related fungus cases had been reported worldwide – of which 70% are said to have arisen in India. With its outbreak since worsening, the number of afflicted patients is now expected to be many folds higher.
Although rare, the black fungus can cause "invasive, life-threatening disease", with spores sometimes extending into a patient's brain.
What is the black fungus?
The black fungus is medically known as mucormycosis, which is made up of several different fungal species.
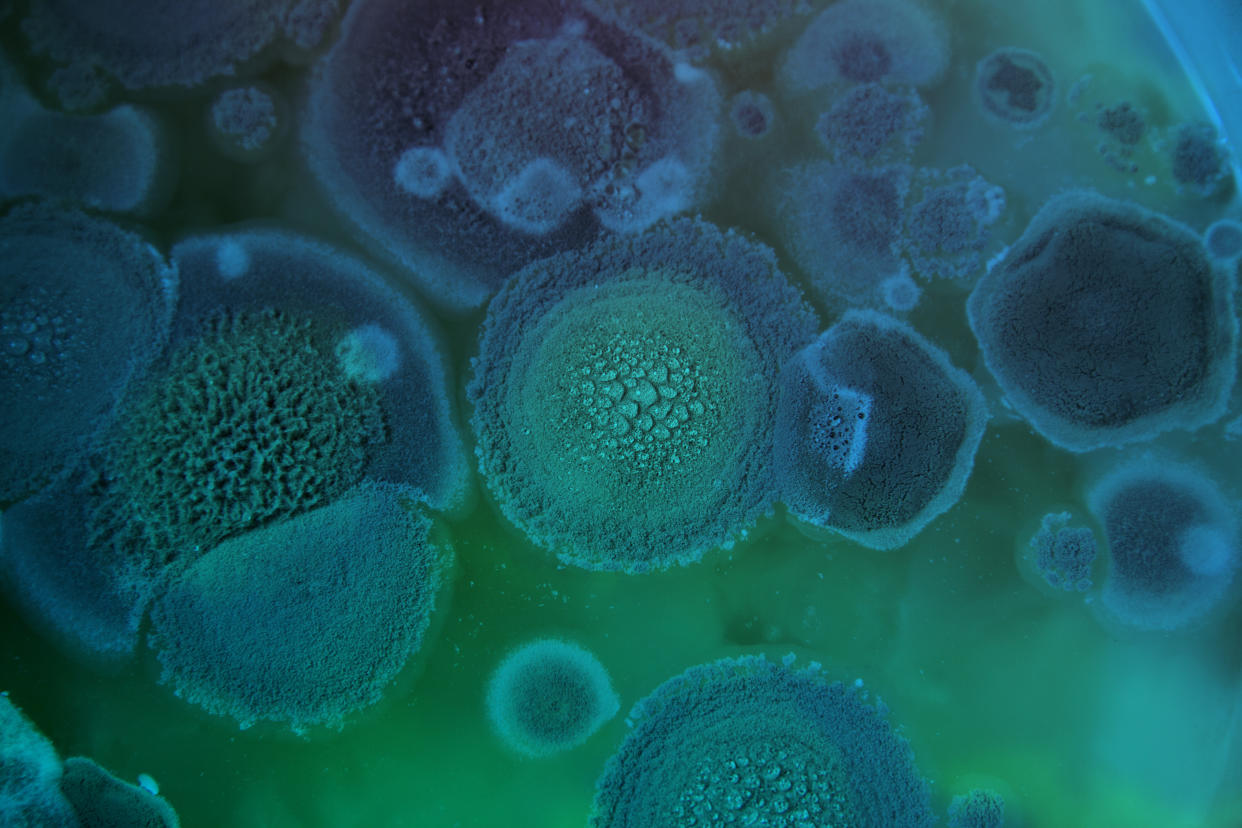
So-called rhizopus is the most common species. In India, however, the apophysomyces species is taking hold. When grown in the laboratory, the fungus has a black-fuzzy appearance.
Mucormycosis species commonly exist in the environment around us.
"Fungi grow in the soil and rotting material like compost, and can produce spores as part of their lifecycle," said Dr Elizabeth Ballou, from the University of Birmingham.
"They become airborne in dry or dusty conditions, or when soil is disturbed."
A healthy person's immune system usually prevents these spores from taking hold.
"The problem comes when patients have suppressed immunity or delayed immunity," said Dr Ballou. "This gives the fungus a chance to grow."
Read more: Optimal coronavirus vaccine for autumn booster investigated
Once the spores have taken hold in a person's body, they can branch off into blood vessels, killing tissues.
"The result can be invasive, life-threatening disease," according to Patient.info.
Although usually inhaled, the spores can also enter the body via wounds, or if swallowed on contaminated food or medicine.
"Fungal infections very rarely pass from person-to-person," said Dr Ballou.
Former UK chief medical officer Professor Dame Sally Davies has reportedly compared this coronavirus complication to cooking a lobster.
Referencing this comment, Dr Ballou said: "While COVID-19 [the disease caused by the coronavirus] is like a lobster going into boiling water, fungal infections are lobsters being brought to a slow boil.
"This is a problem that will slowly creep up on us, but can have just as devastating outcomes if we don't address the root causes."
What are the symptoms?
Inhaled mucormycosis generally takes hold in a patient's nose or sinuses, causing "nasal stuffiness progressing to a black discharge", which may also leak from the palate.
Symptoms tend to be sudden and severe, with many enduring a fever.
Inflamed tissues around the eyes is another early warning sign. The eyeballs may then protrude or ooze, with the eyelid muscles weakening.
As the infection progresses, a patient may develop diplopia – seeing two objects when there is only one – or even sight loss.
In severe cases, the infection can "extend into the brain", causing excruciating headaches on one side or seizures.
Read more: Coronavirus death risk triples among patients battling another airway infection
Once the disease has reached this stage, a patient's outcome tends to be "poor", with many quickly losing consciousness.
Less commonly, the fungus can affect the lungs, leading to breathlessness and coughing.
Skin symptoms can include tissue death that causes black scab-like lesions, which may also secrete a dark discharge.
When caused by malnutrition, mucormycosis can trigger gastrointestinal issues, like pain, bloating, nausea and vomiting.
Watch: What is mucormycosis?
Why is India worst affected?
Pre-pandemic, mucormycosis was also disproportionately high in India, affecting 14 in every 100,000 people versus 0.06 per 100,000 in Australia, for example.
A suppressed immune system can come about due to uncontrolled diabetes or malnutrition, both of which are relatively prevalent in India.
"Even before COVID-19, mucormycosis was more common in India than most countries, partly because of the millions who have diabetes," said Professor Arunaloke Chakrabarti, from the Center of Advanced Research in Medical Mycology in India.
A persistently high blood sugar level, which occurs with uncontrolled diabetes, also makes a patient's tissues more acidic, allowing mucormycosis to thrive.
A recent summary of coronavirus-related mucormycosis revealed more than nine in 10 (94%) patients had diabetes, which was poorly controlled in over two-thirds (67%) of cases.
Writing in the Journal of Fungi, medics from The University of Texas MD Anderson Cancer Center said uncontrolled diabetes and "severe COVID-19" have "converged" to create "the perfect storm for mucormycosis".
Read more: GP opens up about being hospitalised with coronavirus for 5 months
Obesity is also a recognised cause of both type 2 diabetes and severe coronavirus complications. People with both conditions and the infection are therefore more likely to be offered corticosteroids, like dexamethasone.
The inexpensive drug has been shown to cut the risk of death by one third among coronavirus patients on ventilators. Nevertheless, steroid use is known to increase a person's risk of mucormycosis by "dramatically raising blood sugar" levels.
"Mucormycosis is strongly linked to diabetes and diabetes is strongly linked to steroid treatment," said Professor David Denning, from The University of Manchester.
"The remarkable increase in cases in COVID patients, reflects poor diabetes control, worsened by steroids."
When it comes to the coronavirus alone, early research suggests the infection is mild in four in five cases. In severe incidences, however, the lungs can become seriously damaged and the immune system suppressed.
Mucormycosis spores may then take hold in a critically-ill patient's airways or sinuses. Dead or dying tissue similarly creates an acidic environment.
India's climate may also not help matters, with apophysomyces thriving in tropical and subtropical regions.
Watch: Mucormycosis cases rising in India
How is it treated?
More-developed countries have seen an increase in another fungal infection, aspergillosis, among critically-ill coronavirus patients. Similar to mucormycosis, aspergillosis is "opportunistic", taking advantage of an individual's suppressed immune system to invade their body.
According to the Global Action Fund for Fungal Infections, aspergillosis "is present in 5% to 30% of severely-ill COVID-19 patients, regardless of diabetes, further emphasising the caution on excess steroid dose and duration".
Unlike mucormycosis, however, aspergillosis has rapid diagnostics tests, allowing medics to recognise the infection before it can wreak havoc.
Mucormycosis patients tend to have a poor outcome, with "at least 50%" dying and many survivors enduring persistent health complications.
Early diagnosis allows medics to control a diabetes patient's blood sugar, remove dead tissue and administer anti-fungal drugs. This is rarely the case in India, however, with most patients being diagnosed late in the infection's onset.
Even if spotted early, treatment options tend to be limited, with mucormycosis now resistant to many once-effective drugs.
Patients are often given the anti-fungal medication amphotericin B, "and if that doesn't work, unfortunately the only option is surgery to remove the infection," said Dr Ballou.
With India's coronavirus cases continuing to rise, the unprecedented strain on its healthcare systems may make matters worse.
While mucormycosis is very rare in the UK, Dr Ballou has stressed: "Anyone recovering from COVID who is showing symptoms including a bloody or congested nose, pain or numbness in their faces, or blurred vision, should contact their doctor as soon as possible."
Opportunistic infections also make mask-wearing all the more important.
"Anyone recovering from COVID should be cautious about breathing in dust or spores that may cause an infection," said Dr Ballou.
"The good news is clean masks that block COVID will also be effective against fungal spores".



